OFFICE ERGONOMIC
TIPS AND REMINDERS
By Irene Baker, B. of Kin., CCPE, CFCE, MES, COHS
Are you uncomfortable while working at your desk? Do your muscles and joints tend to become aggravated throughout or by the end of the day? If so you may wish to review a few ergonomic tips below. (Ergonomics is the association and interaction between design, arranging equipment safely and the people that use them.)
CAUSE OF INJURY:
Jobs that require you to maintain the same position (i.e. sit or stand) for prolonged periods of time or perform repetitive tasks puts one at a higher risk to developing a muscular skeletal disorder (MSD). MSDs “are injuries that affect muscles, tendons, ligaments and nerves…when the same muscles are used repetitively, or for a long time without adequate rest.” http://www.healthandsafetyontario.ca/Resources/Topics/MSDs.aspx
In addition, MSDs can also be caused by awkward and stressful postures, poor equipment design (i.e. seat too large for smaller female anthropometrics), poor equipment set up (height, depth in relation to worker etc.) MDSs such as tendinitis, carpal tunnel syndrome, repetitive strain injury (RSI) are on the rise (Occupational Safety & Health Administration - OSHA, 2017), as people are using more and more electronic devices including smart phones, tablets etc. in addition to working on their computers 7 to 8 hours per day. The impact of MSDs affecting your neck, shoulders, wrists, back, hips, and lower extremities “account for 43% of all work-related injuries, 43% of all lost-time claim costs, and 46% of all lost-time days. (Source: MOL: Prevention Workplace Pains and Strains! It’s time to take action! Health & Safety Ontario, 2013, http://www.healthandsafetyontario.ca/Resources/Topics/MSDs.aspx)"
PREVENTION:
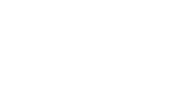
To help prevent or minimize the risks associated with working an office job, we can take a look at our workstations and assess our own stressful postures and equipment set up. Take note of the placement of your items such that you are maintaining neutral postures or avoiding repetitive twisting, rotation, flexion, extension, reaching slouching, cradling telephone between the neck and shoulder, prolonged sitting postures, for 2 hours straight etc.
Ask yourself:
· Is my monitor centered and at the correct viewing height (not looking down or up at the screen, to the right or left all the time)?
· Are my forearms properly supported by the chair's armrests, and at the correct height so my wrists are in the neutral position?
· Are my input devices, mouse and keyboard too far forward (my elbows should be at my sides, not in front of me)?
· Is my mouse in line with my shoulder or off to the side?
· Is my back well supported by my chair?
· Do I have sufficient lumbar support to prevent my pelvis from rotating posteriorly, adding stress on my spine and musculature?
· Are my feet supported so that my thighs are parallel to the ground?
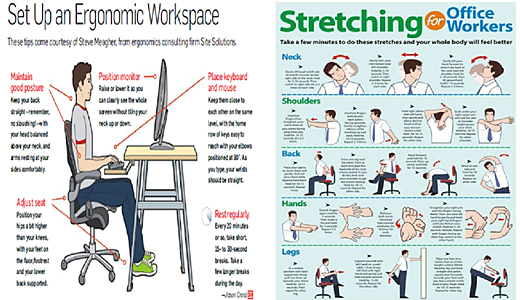
STRETCHING
Be proactive and look out for number one, stretch every 20 - 30 minutes and get up and move, walk around to improve your blood circulation.
Irene Baker, B. of Kin., CCPE, CFCE, MES, COHS is a National Client Relations Manager/Ergonomist at IME Plus Evaluations Ltd. She is a member of the Association of Canadian Ergonomists, has received her Medical Exercise Specialist, Pharmaceutical Representative and Certified Functional Capacity Evaluator certifications. She was also a certified member of the Ontario Kinesiology Association for over 20 years. Irene has recently received her Occupational Health and Safety Certification from Ryerson University. Irene has over 20 years of extensive experience performing physical demands assessments (ergonomic, job-work site, PDAs) in the automobile, disability insurance and employer sectors. She also has experience performing LTD disability case management, return to work programs and implementing temporary and permanent accommodations.